Abstract
Allogeneic stem cell transplantation (HSCT) is the only potential curative treatment for myelodysplastic syndromes (MDS). Non-relapse mortality (NRM) remains a matter of concern despite the introduction of reduced-intensity conditioning in this disease, occurring mainly in an elderly population. Disease features and status at transplant are cornerstones for the risk of relapse. Different pre-transplant parameters have been analysed in various population without resulting in consensus.
Here, we aim to evaluate the predictive role of different pre-transplant parameters including comorbidities on NRM, in 1276 patients who were transplanted for MDS between 2003 and 2014 in centers who participated to the EBMT Data Quality Initiative. The performance of the HCT-CI (Hematopoietic cell transplantation-specific comorbidity index) and PAM (Pretransplant Assessment of Mortality) scores1,2,3 in predicting NRM and overall survival (OS) was investigated according to principles and methods that have been described for external validation of prediction models4. Besides, model discrimination was assessed by the concordance (c) index and its adaptation for competing risks analyses5,6.
Median age was 59 (18-79) and the median follow-up was 73 months. The different scores were categorized as initially published. According to the IPSS classification, two-thirds of the patients were classified within the low or intermediate groups of risk (score ≤1) and one-third within the higher-risk's categories (score ≥1.5). Donors were mostly matched related (34.3%) or unrelated (62.1%), use of peripheral blood stem cells was predominant (89.8%) and conditioning was non-myeloablative in 60% of the transplants. Overall, 731 patients died during the study period, including 445 non-relapse deaths. At 48 months, OS was 46.7% (95%CI 44.0 to 49.6) and NRM was 32.5% (95%CI 29.8 to 35.0).
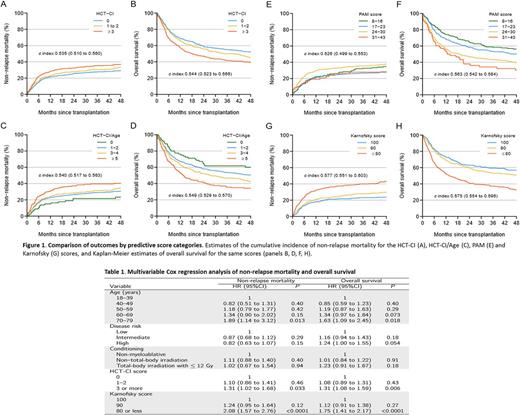
The c-index for HCT-CI score, HCT-CI/Age score and PAM were lower than for Karnofsky score meaning that the scores did not predict better the NRM and the OS than Karnofsky score. Furthermore, PAM score did not predict NRM but was able to predict OS (See Figure 1).
In multivariate analysis including age, disease risk, conditioning, HCT-CI and KS, age ≥ 70 (HR 1.89, 95%CI 1.14-3.12, p=0.013; HR 1.63, 95%CI 1.09-2.45, p=0.018), HCT-CI ≥3 (HR 1.31, 95%CI 1.02-1.68, p=0.033; HR 1.31, 95%CI 1.08-1.59, p=0.006) and KS ≤ 80 (HR 2.08, 95%CI 1.57-2.76, p<0.0001; HR 1.75, 95%CI 1.41-2.17, p<0.0001) were statistically significantly associated with respectively increased risks for NRM and with a decreased OS. Disease risk and intensity of conditioning regimens had no significant influence on outcomes (Table 1).
In conclusion, our study demonstrated on a large homogeneous population of MDS patients the ability of the different comorbidities scoring system to predict toxicity and survival outcomes after HSCT. Among them, Karnofsky score was the most powerful predictive tool. Patient's risk profile assessment is crucial to refine predictive models assessing disease features and transplant procedures.
References: 1. Sorror et al. Blood 2005; 106:2912-2919; 2. Sorror et al. J. Clin. Oncol 2014; 32:3249-3256; 3. Parimon et al. Ann Intern Med 2006; 144:407-414; 4. Royston et al. BMC Medical Research Methodology 2013; 13:33; 5. Harrell et al. JAMA 1982; 247:2543-2546; 6. Wolbers et al. Biostatistics 2014; 15:526-39
Socié: Alexion Pharmaceuticals, Inc.: Consultancy. Kröger: Janssen Global Services, LLC: Speakers Bureau; Amgen Inc.: Speakers Bureau; Novartis AG: Research Funding; RIEMSER Pharma: Research Funding; Neovii Pharmaceuticals AG: Speakers Bureau; Novartis AG: Speakers Bureau; Sanofi: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal